Palliative care improves patient quality of life through the relief of suffering and ongoing attention to what is most important to the patient and family. Palliative care is able to help people live and die in the care setting of their choice with their preferences for who is present, the religious, spiritual, and/or cultural practices they desire, and any important objects they want to have nearby. This is possible through proactive symptom relief, 24/7 availability of palliative care experts and the delivery of palliative care across all care settings.
https://csupalliativecare.instructure.com/courses/
What “best practice” could be in Palliative Care:
SYMPTOMS
- Pain and symptom control
- Control of anxiety and other psychological symptoms (not dying with fear)
- Being assisted by a staff in order to make the process of dying more comfortable
RELATIONAL AND SOCIAL AREA
- Respect of cultural values and individual preferences
- Emotional support provided to the family
- Good communication among patient/families/close friends/caring staff
- Having close people nearby/family acceptance of the patient’s condition/not feeling a burden for family and friends
PREPARATION
- Importance given to preparation/awareness of diagnosis/awareness of dying
- Choice of place of dying
- Maintaining a sense of control (the possibility of controlling relevant aspects of one’s own existence and/or deciding what and when to delegate to others); maintaining a dimension of continuity of life right to the end
EXISTENTIAL CONDITION
- Being at peace with oneself/finding meaning
- Spiritual needs/Religious practices
END-OF-LIFE DECISIONS
- Death as natural or normal/Not to hasten nor to postpone death
- Death as an unwanted effect of sedation/Withdrawing or withholding treatments/Euthanasia and assisted suicide
- Participation in the decision-making process
QUALITY OF LIFE
DIGNITY
Barazzetti et al. BMC Palliative Care 2010, 9:1
http://www.biomedcentral.com/1472-684X/9/1
No one knows the exact time or place of his or her death.
In the final days, the body’s letting go
increases in intensity effecting all organs and systems.
Nothing is left unaffected.
Once understood, physical death no longer needs to be feared
rather it can once again be seen
as a natural part of the life cycle.
Every one of us will experience death, no exceptions.
https://pubmed.ncbi.nlm.nih.gov/21357182/
THE ROLE OF SOCIAL WORKERS
IN PALLIATIVE, END OF LIFE AND BEREAVEMENT CARE
Palliative care social workers take a lead to:
☛ Support people and communities to make their voices heard and to achieve what is important to them at end of life and in bereavement
☛ influence all organisations responsible for providing palliative, end of life and bereavement care to adopt an approach of co-production with people who have lived experience
☛ Support all agencies and communities to respond to people’s needs
☛ Participate in and lead key discussions around service delivery in end of life and bereavement care
☛ Take up senior practice and management roles, and encourage more organisations to appoint social workers at this level
☛ Negotiate changes in working practices to improve collaboration between services
☛ Enhance the evidence base for, and learning and development in, palliative, end of life and bereavement care
☛ Use evidence to identify unmet need and improve service provision
☛ Teach and mentor others
☛ Look after themselves and support other members of the team in dealing with dying, death and bereavement.
Specialty palliative care: “Palliative
care that is delivered by health care professionals who are palliative
care specialists, such as physicians who are board certified in this
specialty; palliative-certified nurses; and palliative care-certified
social workers, pharmacists, and chaplains.”
Primary palliative care (also known as generalist palliative care): “Palliative
care that is delivered by health care professionals who are not
palliative care specialists, such as primary care clinicians; physicians
who are disease-oriented specialists (such as oncologists and
cardiologists); and nurses, social workers, pharmacists, chaplains, and
others who care for this population but are not certified in palliative
care.”
https://web.archive.org/web/20200214132437/https://nationalcoalitionhpc.org/wp-content/uploads/2018/10/NCHPC-NCPGuidelines_4thED_web_FINAL.pdf
https://www.nationalcoalitionhpc.org/ncp/
- Depression – sad or blue
- Anxiety – nervousness or restlessness
- Tiredness – decreased energy level (but not necessarily sleepy)
- Drowsiness – sleepiness
- Well-being – overall comfort, both physical and otherwise; truthfully answering the question “How are you?”
Advance Healthcare Directive can cover:
Pain management:
To what extent you would like to be treated for pain to ensure that you are comfortable and that your dignity is maintained.
Artificial life support:
In which instances you would like to refuse artificial life support, even if it means hastening the moment of death.
Organ and tissue donation:
Whether you would like to donate your organs and tissues, including the donation of your body for medical study and research.
Brain autopsy:
In the case of dementia, you may grant permission for a scientific examination of the brain tissue after death which may provide valuable insight for doctors and researchers.
Aggressive medical care:
You may wish to request aggressive medical and treatment to prolong your life even if you are suffering from a terminal illness.
Feeding tubes:
You can indicate whether to permit or refuse feeding tubes, such as PEG tubes, NB tubes or central intravenous lines, in the event that you cannot swallow or eat. Bear in mind that feeding tubes can cause infections and complications. You can also express your wish to refuse manual force feeding by a care giver.
IV hydration:
You may wish to refuse IV hydration if you are unable to drink, bearing in mind that this can be uncomfortable and can cause difficulty breathing.
CPR:
In your advance directive you can decline CPR which will means that a do-not-resuscitate (DNR) sign will be placed on your medical chart.
Electrical, mechanical or other artificial stimulation of the heart:
You may expressly permit or refuse such interventions.
Palliative care:
You can include your wishes regarding palliative care, hospice and the treatment of pain. You can include details on where you would prefer to be cared for and by whom.
Antibiotics:
You may wish to refuse all antibiotics outright or permit then only in instances to control symptoms and pain management.
Blood transfusion:
Your advance directive can include your request to either permit or refuse a blood transfusion.
Because an advance directive must be drafted while a person still has legal capacity, in the case of a dementia diagnosis, the document should be drafted as soon as possible and before the disease progresses.
https://crue.co.za/advance-directive-your-voice-when-yours-is-silenced/
COURSE IN
PALLIATIVE
MEDICINE
A MANUAL
https://web.archive.org/web/20211010142328/http://s3-eu-west-1.amazonaws.com/cairdeas-files/76/foundation_course_in_palliative_medicine_-__a_manual.pdf
- Pain and Symptom Management
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx#tabs-2504
- Functional Status
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx#tabs-2507
- Psychosocial Care
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx#tabs-2510
- Caregiver Assessment
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx#tabs-2513
- Quality of Life
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx#tabs-2516
Patients with life limiting illness may develop a number of symptom issues as their disease advances therefore as health practitioners anticipate and manage these problems awareness of the impact of total suffering is crucial.
- Opioids are the drug of choice for both pain and dyspnea in advanced disease.
- Patients with addiction should have pain/dyspnea treated — use long acting opioid medications, limited breakthroughs, small amount dispensed frequently.
- Opioids are safe in cardiopulmonary disease, but start low go slow.
- Persistent symptoms require regular dosing, i.e. short-acting opioid q4 hours.
- Not all opioids are the same, and inter-individual analgesia/side effects vary widely.
- Opioids with few or no active metabolites are preferred for those with renal failure or frailty.
- Always order breakthrough with regular dosing: 10% of total daily opioid dose q1h prn. Recalculate breakthrough dose when regular dose is changed.
- If 3 or more breakthroughs used in the last 24 hours, increase the regular dose.
- Titrate dose to the best symptom control with the fewest side effects.
- When you prescribe an opioid, prescribe a laxative.
- If side effects are intolerable, consider rotating opioid.
- Educate patient/family about control of symptoms and opioid safety.
Five Steps of Advance Care Planning
An Advance Health Care Directive is a legal document that tells your physician, your family members and friends about what kind of care you would like to have if you become unable to make medical decisions. It's called an advance directive because you choose your medical care before you become seriously ill.
https://www.psjhmedgroups.org/Orange-County/Patients-Families/Advance-Care-Planning.aspxAn advance directive also allows you to express your values and desires related to end-of-life care. You might think of it as a living document—one that you can adjust as your situation changes because of new information or a change in your health.
https://www.nia.nih.gov/health/advance-care-planning-healthcare-directives
Advance Care Planning is a process of reflection and communication. It is a time for patients to reflect on their values and wishes, and to let loved ones know what kind of health and personal care is desired in the future. It is intended to address the question: What if something happens?
https://library.nshealth.ca/PalliativeCare/Plan
The Advance Care Directive Do-It-Yourself Kit includes the Advance Care Directive Form and a step-by-step guide that has everything you need to know to complete your Advance Care Directive. This includes example statements, information for substitute decision-makers, witnesses and interpreters, fact sheets and other resources.
http://www.advancecaredirectives.sa.gov.au/
Downloading Your Advance Directive
Advance care planning forms
Advance care planning is about your future health care. It gives you the opportunity to plan for what you would want or not want, if you become unable to make or communicate your own preferences.
The following outlines the legal requirements, forms and fact sheets in Victoria (VIC):
https://www.advancecareplanning.org.au/resources/advance-care-planning-for-your-state-territory/vic#/
Advance Care Directive Formhttps://advancecaredirectives.sa.gov.au/upload/home/ACDForm_Handwritten.pdf
- 1. Your Substitute Decision-Maker? ...
- 2. What is important to you? ...
- 3. Outcomes of care you wish to avoid? ...
- 4. Health care you prefer? ...
- 5. Where you wish to live? ...
- 6. Other personal arrangements? ...
Sample Advance Directive Form
What is Palliative Care?
Advance Care Planning (ACP)
is really just planning ahead.
Most of us won’t die suddenly.
We’ll develop an illness
or a long-term health condition
(or more than one, especially if we live long enough)
and our health will gradually deteriorate.
Most of us will manage that process surprisingly well:
we’ll find new ways to do things we enjoy,
we’ll take different pleasures,
and life will still feel sweet even
if it’s more limited
than it used to be.
We humans are very resilient.
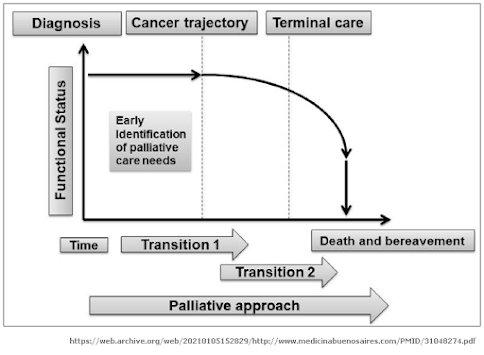
The first clinical trajectory,
typically associated to cancer,
features a stable and/or low decline phase
broken up by a severe decline in the last weeks.
Asking questions to recognize end of life transitions could be:
Transition 1:
Would my patient benefit from supportive and palliative care?
Transition 2:
Is my patient reaching the last days of life?
https://web.archive.org/web/20210105152829/http://www.medicinabuenosaires.com/PMID/31048274.pdf
Moving from pallilalia ( all talk, no actions) to Palliactive:
— Eduardo Bruera MD (@edubru) June 24, 2021
1. Every hospital with an ICU has a PCU
2. Self-standing supp and pall care outpatient center
3. Every medical school and hospital has a Department of suppo and pall care. #hpm #PalliativeCare
Palliative and End of Life Care Strategy - ENHCCG-Palliative-and-End-of-Life-Strategy-FINAL.pdf
https://www.enhertsccg.nhs.uk/sites/default/files/documents/Oct2017/ENHCCG-Palliative-and-End-of-Life-Strategy-FINAL.pdf
EOLC strategy Aug 2015 FINAL - EOLC-strategy-Aug-2015-FINAL.pdf
https://www.wsh.nhs.uk/CMS-Documents/Corporate-information/EOLC-strategy-Aug-2015-FINAL.pdf
end-of-life-care-vision-and-strategy-version-v7-7-final.pdf
https://www.hct.nhs.uk/media/1633/end-of-life-care-vision-and-strategy-version-v7-7-final.pdf
51636-End-of-Life-Care-16pp-final.pdf
https://www.dchs.nhs.uk/assets/public/dchs/dchs_about_us/End-Of-Life-Care/51636-End-of-Life-Care-16pp-final.pdf
EOL-strategy-FINAL.pdf
https://www.westernsussexhospitals.nhs.uk/wp-content/uploads/2014/12/EOL-strategy-FINAL.pdf
ELCNewsletter6_FINAL.pdf
https://www.gloucestershireccg.nhs.uk/wp-content/uploads/2012/03/ELCNewsletter6_FINAL.pdf
ncpc-mca-final.pdf
https://www.scie.org.uk/files/mca/directory/ncpc-mca-final.pdf?res=true
MCN-Annual-Report-FINAL.pdf
https://leedspalliativecare.org.uk/wp-content/uploads/2019/05/MCN-Annual-Report-FINAL.pdf
12 Appendix 1 Cwm Taf End of Life Delivery Plan v4 FINAL - 12 Appendix 1 Cwm Taf End of Life Delivery Plan v4 FINAL.pdf
http://www.cwmtafuhb.wales.nhs.uk/sitesplus/documents/865/12%20Appendix%201%20Cwm%20Taf%20End%20of%20Life%20Delivery%20Plan%20v4%20FINAL.pdf
Okay kan, Bro!
IKA SYAMSUL HUDA MZ