It improves quality
of life.
It can be given in
homes, health
centres, hospitals
and hospices.
It is care for patients with
life-threatening illnesses
& their families.
It benefits health systems
by reducing unnecessary
hospital admissions.
It relieves physical,
psychosocial &
spiritual suffering.
It can be done by many types
of health professionals &
volunteers.
https://web.archive.org/web/20200824024241/https://www.who.int/ncds/management/palliative-care/Infographic_palliative_care_EN_final.pdf
Palliative care is based on a model developed in response
to the needs of cancer patients by the hospice movement in the UK.
Such treatment, while not curative, nevertheless prolongs life
for considerable periods of time and restores quality of life.
https://www.who.int/3by5/en/palliativecare_en.pdf
Support for caregivers
is an essential part of palliative care,
whether they be family members
or professional carers.
For professional carers,
an integral part
of providing palliative care
is to work with families and friends
to ensure effective communication.
https://web.archive.org/web/20200816120954/https://www.who.int/3by5/en/palliativecare_en.pdf
a patient’s experience with cancer.
It should begin at diagnosis
and continue through treatment,
follow-up care,
and the end of life.
WHO GIVES PALLIATIVE CARE?
may provide palliative care
by addressing the side effects
and emotional issues of cancer,
some have a particular focus
on this type of care.
A palliative care specialist is
a health professional who specializes
in treating the symptoms,
side effects,
and emotional problems
experienced by patients.
The goal is to maintain
the best possible quality of life.
Often, palliative care specialists work
as part of a multidisciplinary team
to coordinate care.
This palliative care team may
consist of doctors,
nurses,
registered dieticians,
pharmacists,
and social workers.
Many teams include psychologists
or a hospital chaplain as well.
Palliative care specialists
may also make recommendations
to primary care physicians
about the management of pain
and other symptoms.
People do not give up
their primary care physician
to receive palliative care.
https://web.archive.org/web/20210516114044/https://www.cancercareontario.ca/sites/ccocancercare/files/assets/ACCUPalliativeCare.pdf
https://www.nottinghamshire.gov.uk/owl/learning/resources-all-providers/end-of-life
Here we discuss the common medicines used in syringe drivers to treat these symptoms. All medicines can cause side effects, so it’s a good idea to check what to expect with your doctor or nurse before taking them. A specialist doctor or nurse may also suggest other drugs to control difficult symptoms.
- http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2017/08/PETUNJUK_TEKNIS_PROGRAM_PALIATIF_KANKER_ANAK.pdf
- http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2017/08/PETUNJUK_TEKNIS_PALIATIF_KANKER_PADA_DEWASA.pdf
- http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2017/08/PEDOMAN_NASIONAL_PROGRAM_PALIATIF_KANKER.pdf
- http://p2ptm.kemkes.go.id/uploads/VHcrbkVobjRzUDN3UCs4eUJ0dVBndz09/2017/08/MODUL_TOT_PALIATIF_KANKER_BAGI_TENAGA_KESEHATAN.pdf
There are currently three programmes of research: each focused on people affected by cancer, other life limiting illnesses, and those requiring end of life care:
https://www.southampton.ac.uk/chp/research/endoflife.page
Management of Lymphoedema in Palliative Care
Lymphoedema occurs due to the inability of the lymphatic system to maintain normal tissue homeostasis. This results in an accumulation of protein-rich fluid in the subcutaneous tissues.
Lymphoedema is one form of chronic oedema.
In patients with cancer, lymphoedema is often secondary to the underlying cancer or previous cancer treatment.
Where available, patients should be referred to specialist lymphoedema clinics
The core treatment elements are:
- • Skin care – keep skin intact, clean and well hydrated with non-perfumed emollient (e.g, Diprobase®, Doublebase® or Zerobase®)
- • Compression/support stockings
- • Movement and exercise
- • Simple lymph drainage, self-massage techniques.
- • Avoid affected limb for any medical procedure where possible, e.g injection, venepuncture, blood pressure measurement
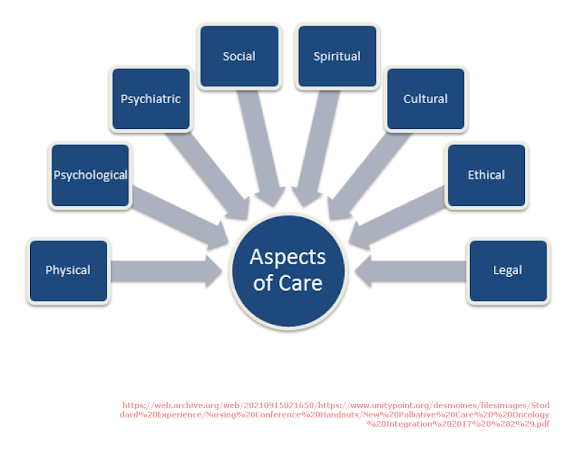
The concept of “total pain” or “total suffering” indicates that there are many factors which contribute to the experience of pain and other physical symptoms and each patient must be treated with the knowledge that physical symptoms cannot be treated in isolation. Whatever symptom a patient is experiencing it is important to look at it in the context of the above diagram which describes the concept of total suffering.
http://mobcdhb.palliativecare.org.nz/Total%20Suffering.pdf
Primary care professionals play a huge role in the care of people affected by cancer. We have developed an exciting new cancer resource for whole practice teams – the Macmillan Cancer Quality Toolkit for Primary Care (Wales). It is designed to support practices to review cancer services and make changes to help deliver improved person-centred care to the increasing number of people affected by cancer in Wales.
http://www.primarycareone.wales.nhs.uk/macmillan-cancer-quality-toolkit
Poor communication, planning, pain management and co-ordination lead to tragic and avoidable suffering.
Anticipatory prescribing and ‘just in case’ boxes are an important part of end-of-life care. Anticipatory prescribing enables prompt symptom relief at whatever time the patient develops distressing symptoms.
- 1. Ensures there is a supply of drugs in the patient’s home
- 2. Ensure they have the apparatus needed to administer them
- 3. Ensures both are available to an attending clinician for use where appropriate
- 4. These drugs belong to the patient, and have the same legal status as other prescribed controlled drugs.
Signs of pain include:
- Noisy breathing – labored, harsh, or rapid breaths
- Making pained sounds – including groaning, moaning, or expressing hurt
- Facial expressions – looking sad, tense, or frightened; frowning or crying
- Body language – tension, clenched fists, knees pulled up, inflexibility, restlessness, or looking like they’re trying to get away from the hurt area
- Body movement – changing positions to get comfortable but can’t
Assessment forms can ensure that:
-
Assessments are routinely completed as a suite at each assessment occasion.
- Assessment scores are documented or recorded at point of care.
https://ahsri.uow.edu.au/pcoc/forms/index.html
Prescribing Anticipatory Drugs
‘Anticipatory’ drugs in a palliative setting are those drugs that are prescribed for use on an ‘as required’ basis to manage common symptoms that can occur at the end of life. In most cases these drugs will be prescribed as a subcutaneous injection and will usually include four key drugs: an opioid (for management of pain or breathlessness), an antiemetic, an antisecretory drug (for respiratory secretions) and a sedative.
Readily available anticipatory drugs can prevent inappropriate readmissions to hospital. It is especially important to ensure that drugs are available over weekends and bank holidays.
https://web.archive.org/web/20200720092733/https://www.northkirkleesccg.nhs.uk/wp-content/uploads/2013/07/Guidance-on-Prescribing-Anticipatory-Drugs-and-Syringe-Drivers-in-the-Community.pdf
Australia-modified Karnofsky Performance Status (AKPS)
A conceptual framework toward understanding “actively dying,” “end of life,” “terminally ill,” “terminal care,” and “transition of care.” Based on our systematic review, end of life, terminally ill, and terminal care period are synonymous and apply to patients with progressive disease with months or less of expected survival. Actively dying is related to patients with days of survival, and transition of care is related to changes in the place of care, level of care, and goals of care.
https://www.jpsmjournal.com/article/S0885-3924(13)00243-1/fulltext#sec3.3
PLEURAL EFFUSION TREATMENT IN PALLIATIVE CARE
https://pharmacopallcare.blogspot.com/2020/09/pleural-effusion-treatment-in.html
Morphine Sulfate 10mg/ml Injection BP
- Morphine Sulfate may be given by the subcutaneous, intramuscular or intravenous route. The subcutaneous route is not suitable for oedematous patients. The dosage should be based on the severity of the pain and the response and tolerance of the individual patient. The epidural or intrathecal routes must not be used as the product contains a preservative.
- Prior to starting treatment with opioids, a discussion should be held with patients to put in place a strategy for ending treatment with morphine sulphate in order to minimise the risk of addiction and drug withdrawal syndrome
https://www.capc.org/about/press-media/press-releases/2010-1-6/palliative-sedation-myth-vs-fact/
The more common side effects that can occur with dexamethasone oral tablets include:
- nausea
- vomiting
- stomach upset
- swelling (edema)
- headache
- dizziness
- mood changes, such as depression, mood swings, or personality changes
- trouble falling asleep
- anxiety
- low potassium levels (causing symptoms such as tiredness)
- high blood glucose
- high blood pressure
https://www.healthline.com/health/dexamethasone-oral-tablet#side-effects
BMC Palliative Care
http://www.biomedcentral.com/bmcpalliatcare/
BMJ Supportive Palliative Care
Current Opinion in Supportive and Palliative Care
http://journals.lww.com/co-supportiveandpalliativecare/pages/currenttoc.aspx
Family Practice Palliative Care
HIV/AIDS - Research and Palliative Care
http://www.dovepress.com/hivaids---research-and-palliative-care-journal
Indian Journal of Palliative Care
http://www.jpalliativecare.com/currentissue.asp
Journal of Geriatrics and Palliative Care
http://www.avensonline.org/medical/journal-of-geriatrics-and-palliative-care/home-10
Journal of Pain Palliative Care Pharmacotherapy
http://www.tandfonline.com/loi/ippc20
Journal of Social Work in End-of-Life Palliative Care
http://www.tandfonline.com/loi/wswe/
Palliative Supportive Care
https://www.cambridge.org/core/journals/palliative-&-supportive-care
Palliative Care Social Practice
https://journals.sagepub.com/home/pcr
Palliative Care: Research and Treatment
http://journals.sagepub.com/home/pcr
Progress in Palliative Care
http://www.tandfonline.com/loi/yppc20
WHAT IS PALLIATIVE CARE ?
Pediatric Palliative Care Approach to
Pain & Symptom Management
2020
https://web.archive.org/web/20200910094138/https://pinkbook.dfci.org/assets/docs/blueBook.pdf
Show an interest in the patient’s symptoms.
Many patients with advanced cancer believe
that suffering is an inevitable part
of the disease or of its treatment.
Ask patients about their symptoms
in a positive and detailed fashion,
starting with open-ended questions
and following up with specific questions.
Patients may underreport their symptoms
or may not mention them
if not asked directly.
https://www.ccjm.org/content/78/1/25
Ookay kan, Bro!