Five Wishes lets your family and doctors know:
1. Who you want to make health care decisions for you when you can’t make them.
2. The kind of medical treatment you want or don’t want.
3. How comfortable you want to be.
4. How you want people to treat you.
5. What you want your loved ones to know.
https://samaritannj.org/resources/5-wishes-living-will-documents/
An advance health care directive is a document in which a person sets out his or her wishes regarding future health care decisions. These might include consent, refusal to consent, or withdrawal of consent for any care, treatment, service, or procedure to maintain, diagnose, treat, or provide for an individual’s physical or mental health.
Advance Health Care Directive
https://healthy.kaiserpermanente.org/southern-california/health-wellness/life-care-plan/advance-health-care-directive#enableScroll
Health Care Directive
https://www.lawdepot.com/ie/estate/living-will-medical-power-of-attorney/preview.aspx?loc=IE&
A set of 6 short audio films talking about End of Life and Dying issues during COVID-19 from the Muslim perspective. The aim of these is to help answer questions of mistrust and misconceptions around people dying from coronavirus, especially admission into hospital.
https://updatebrum.co.uk/c19supportbrum/six-short-audio-films-about-end-of-life-and-dying-issues-from-the-muslim-perspective/
Communication
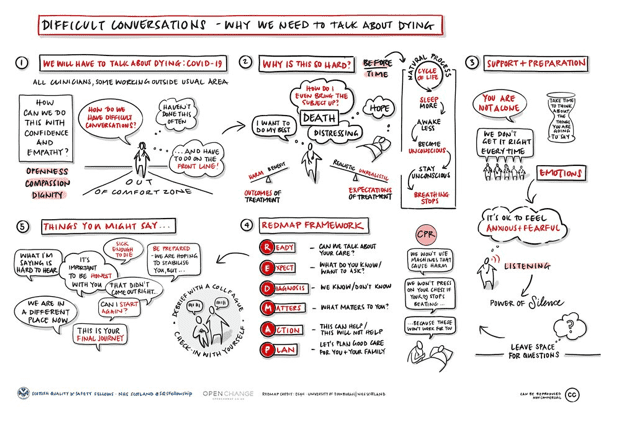
Difficult conversations – why we need to talk about dying

https://www.multiplechronicconditions.org/palliative-care
PALLIATIVE CARE SHOULD BE AVAILABLE TO PEOPLE EARLIER
Many agreed that the benefits
of palliative care should be
available to people earlier
in the progression of their disease.
From 2012 some studies even showed
increased survival among those
who received palliative care.
There was also a strong desire
to move beyond cancer,
the disease that had defined
the approach of the hospice pioneers.
Areas of further palliative care specialisation
began to appear – in
cardiology,
renal medicine,
stroke,
respiratory disease
and neurological conditions.
The medical model of palliative care was
gathering strength.
Likewise, domains of
‘general’,
‘specialised’
and ‘specialist’
palliative care came
to be characterised
according to the complexity
of the problems encountered
and the skills needed
to address them.
Those who focussed
on palliative care
for older people (‘geripal’)
stepped up to the plate
and paediatric palliative care
gathered its own momentum.
Palliative care according
to setting (hospital or community based)
came to be differentiated.
http://endoflifestudies.academicblogs.co.uk/controversies-in-palliative-care-a-matter-of-definition/
Palliative care helps with personal, social and medical problems associated with potentially mortal illness, especially pain and other distressing symptoms. It assists families and carers and supports them in bereavement. It uses skilled approaches from a trained team, but often involves friends, family members and the wider community. Palliative care improves wellbeing and in some instances has even been shown to extend life”.
(David Clark 18 January 2019 - http://endoflifestudies.academicblogs.co.uk/controversies-in-palliative-care-a-matter-of-definition/)
http://endoflifestudies.academicblogs.co.uk/controversies-in-palliative-care-a-matter-of-definition/
The main disease groups identified as needing palliative care are:
- advanced cancers
- end stage organ failures (heart failure, respiratory disease, renal failure, and liver failure)
- neurodegenerative diseases, such as motor neurone disease, multiple systems atrophy, Parkinson's disease, Huntington's disease
- advanced dementia/Alzheimer's
- https://meteor.aihw.gov.au/
- https://apps.hnehealth.nsw.gov.au/
- https://ahsri.uow.edu.au/
- https://www.wnswphn.org.au/
- Five Phases of Palliative Care
https://www.wnswphn.org.au/ - An episode of admitted patient palliative care may comprise a single phase or multiple phases, depending on changes in the patient's condition. Phases are not sequential and a patient may move back and forth between phases within the one episode of admitted patient palliative care.
http://www.npcrc.org/content/25/Measurement-and-Evaluation-Tools.aspx
The principles of good end of life care are:
- ☛ Effective communication with patients and their families
- ☛ Regular assessment
- ☛ Management of symptom control
- e.g. ensure anticipatory medications prescribed
- ☛ Avoid unnecessary interventions
- e.g. ensuring DNACPR status, the need for ongoing observations/investigations/blood tests reviewed
- ☛ Provision of psychological, social and spiritual support
- ☛ Food/fluids as desired – may be appropriate for comfort even if unsafe swallow. Parenteral fluids may be continued/commenced if appropriate.
https://www.gloshospitals.nhs.uk/documents/9696/Guidance_for_symptom_control_in_EOL_5EI23V1.pdf
☀☀☀
The Psychosocial Assessment in Palliative
Patient’s thoughts and feelings about illness, treatment, and care.
- a. What do we need to know about you and your family to give you the best care?
- b. How do you and your family best receive information?
- c. What is most important to you right now? And as you think about the future? Is this different from what you perceive as important to your family?
Coping with emotions, functional changes, symptoms etc.
- a. What have been the most significant changes in your life?
- b. How does illness and symptoms affect your everyday life?
- c. What does the future look like to you?
- d. What substances (e.g., alcohol, marijuana, opioids, and cocaine) have you used or experimented with in the past? Have you ever used these substances to cope with unwanted feelings?
Cultural influences
- a. How do you understand what is happening to your health?
- b. What cultural or ethnic group do you identify with?7
- c. What is your preferred language? What primary language is spoken at home?
- d. Have you been able to maintain contact with family or friends from your country of origin? Have you any plans for visiting that family now or in the future?
- e. (If appropriate to the patient’s awareness) Where is your preferred place of death?
Social context
- a. Who is your family? Of origin and of creation?
- b. How would you prefer to be addressed? Preferred pronoun?
- c. Where do you live? Do you live alone or with others? Are there timeswhen you think about if/when you need more assistance at home andwhat thatmight look like?
- d. Are you a veteran?
- e. Are you currently employed?
Lived experience of illness, impact on self, others, and quality of life.
- a. Do you worry about the financial impact or how your health expenses will be covered?
- b. What has been the impact of this illness on your work and those important to you?
- c. What or whom are you concerned about with regard to your health?
- d. What have you shared about your illness with family and friends?
- e. Who can help with decision making? Who do you go to when things get tough? Do you have a health care power of attorney or agent? Who might have copies of those documents?
- f. Have you, or those close to you, managed serious illness before? Any recent losses?
- g. (If appropriate to the patient’s prognostic awareness) Have you made funeral or after-death plans? Plans for cremation or burial here or in country of origin?
Suffering and the existential/spiritual domain
- a. Are religious or spiritual beliefs or rituals important to you?
- b. Are you being supported by a spiritual community? Does your illness allow you to still access this support? If not, can this support come to you—in person or through technology?
- c. What brings you comfort?
- d. How does this illness influence your thoughts and relationship to your god or a higher power?
- e. Do you feel at peace?
https://europepmc.org/article/MED/32790573
☀☀☀








