Saya akan bertanggungjawab di hadapan Tuhan tentang Perawatan Paliatif dan Akhir Hayat,
Saya tidak bertanggungjawab tentang kesembuhan pasien kanker yang dengan diagnosis yang tidak tepat dan terlambat, dan tidak mendapatkan anti kanker yang adekuat.
Despite the universality of death,
much research has not focused
on the unique needs
of dying persons and their families.
Those of us who care for
and study the dying are
often facing uncharted waters.
As noted by Dame Cicely Saunders,
we must be committed to sharing knowledge,
open to challenging fundamental assumptions,
and willing to recognize that
the key to quality of medical care
for the dying is the dying person’s
and his/her family’s
“own view on what they need.”
Recognising dying is
marred by prognostic uncertainty.
This complex clinical decision
commonly relies on the skill
and experience of the clinician,
which can be complemented
by clinical tools developed
to assist in recognising
the dying patient
and avoiding potentially harmful
and futile treatments.
The specifics of a ‘good death’ vary for each individual and defy neat definition.
- To know when death is coming, and to understand what can be expected.
- To be able to retain control of what happens.
- To be afforded dignity and privacy.
- To have control over pain relief and other symptom control.
- To have choice and control over where death occurs (at home or elsewhere).
- To have access to information and expertise of whatever kind is necessary.
- To have access to any spiritual or emotional support required.
- To have access to hospice care* in any location, not only in hospital.
- To have control over who is present and who shares the end.
- To be able to issue advance directives which ensures wishes are respected.
- To have time to say goodbye, and control over other aspects of timing.
- To be able to leave when it is time to go, and not to have life prolonged pointlessly.
EARLIER IDENTIFICATION:
Individuals who have a progressive,
life-limiting illness should have
their palliative care needs
identified early
through a comprehensive
and holistic assessment.
The initiation of palliative care should not
be determined by prognosis;
it can begin as early as the time of diagnosis,
and it can be provided alongside treatment.
Earlier identification is
a deliberate proactive decision point
in a person’s health care journey.
The process should include
assessing patient and families’ needs
across multiple domains
including physical,
psychosocial-spiritual,
grief and loss.
At this point,
open and honest communication
with the individual
and their family is
essential,
and should include
initiation of
goals of care discussions.
Electronic Proactive Assessment and Information Guide for End of Life (EPaige)
http://www.cheshire-epaige.nhs.uk/
Care at the end of life
https://www.health.qld.gov.au/clinical-practice/guidelines-procedures/patient-safety/end-of-life
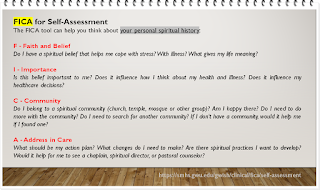
FICA for Self-Assessment
https://smhs.gwu.edu/gwish/clinical/fica/self-assessment
The FICA tool can help you think about your personal spiritual history:
F - Faith and Belief
Choosing where you would like to die is a personal decision. Here we outline the options of dying in your own home, in a palliative care unit or hospice, in hospital, or in a residential aged care facility.
Tiga pemicu yang menunjukkan bahwa pasien mendekati akhir hidup adalah:
- Pertanyaan Kejutan: "Apakah Anda akan terkejut jika pasien ini mati dalam beberapa bulan, minggu, hari berikutnya"?
- Indikator umum penurunan - kemunduran, meningkatnya kebutuhan atau pilihan tanpa perawatan aktif lebih lanjut.
- Indikator klinis spesifik terkait dengan kondisi tertentu.
THE GSF - PROGNOSTIC INDICATOR GUIDANCE
https://www.goldstandardsframework.org.uk/cd-content/uploads/files/General%20Files/Prognostic%20Indicator%20Guidance%20October%202011.pdf
A MODEL TO GUIDE HOSPICE PALLIATIVE CARE
© Canadian Hospice Palliative Care Association, Ottawa, Canada, 2013
Perawatan paliatif memainkan peran penting bagi pasien selama sakitnya, tidak hanya pada akhir kehidupan. Pengobatan penyakit menurun seiring dengan perkembangan penyakit, sementara perawatan paliatif meningkat ketika orang tersebut mencapai akhir kehidupan. Perawatan paliatif juga memberikan dukungan bagi keluarga selama seluruh masa ini. Setelah pasien meninggal, penting untuk memberikan konseling berkabung untuk keluarga dan teman-teman.
http://bc-cpc.ca/cpc/documents/pdf/Chapter%201-%20Palliative%20Care%20is%20a%20Public%20Health%20Issue.pdf
INTERNATIONAL ASSOCIATION FOR HOSPICE AND PALLIATIVE CARE (IAHPC) LIST OF ESSENTIAL DRUGS FOR PALLIATIVE CARE
http://inctr-palliative-care-handbook.wikidot.com/iahpc-list-of-essential-drugs-for-palliative-care
END OF LIFE CARE FOR ADULTS
- People approaching the end of life are identified in a timely way.
- People approaching the end of life and their families and carers are communicated with, and offered information, in an accessible and sensitive way in response to their needs and preferences.
- Orang yang mendekati akhir kehidupan ditawarkan penilaian holistik komprehensif dalam menanggapi perubahan kebutuhan dan preferensi mereka, dengan kesempatan untuk membahas, mengembangkan dan meninjau rencana perawatan yang dipersonalisasi untuk dukungan dan perawatan saat ini dan di masa depan.
- ...
Anticipatory Care Planning is about helping people think ahead. ACP is a process that helps people make choices about their future care. ACP is also about knowing how to use services better. Planning ahead can help people to be more in control and more able to manage changes in their health and wellbeing. It also helps people tell others about what matters most to them.
https://www.ec4h.org.uk/resources/anticipatory-care-planning-in-scotland/
A Model to Guide Hospice Palliative Care:
Based on National Principles and Norms of Practice
Revised and Condensed Edition: 2013
Perawatan paliatif paling efektif diberikan oleh tim interprofesional penyedia layanan kesehatan yang berpengetahuan luas dan terampil dalam semua aspek perawatan dalam disiplin praktik mereka. Tim profesional datang bersama dengan anggota keluarga, teman dan pengasuh lainnya untuk membentuk lingkaran peduli di sekitar orang dan keluarga.
https://www.chpca.ca/wp-content/uploads/2019/12/norms-of-practice-eng-web.pdf
In hospitals – research would suggest that at any one time 30% of acute hospital inpatients will be in their final year of life (Clarke 2014).
https://www.goldstandardsframework.org.uk/How-to-use-the-GSF-PIG-in-your-practice
Discussing Values, Goals, and Preferences
https://sites.google.com/view/10-tips-for-prescribingeolc/discussing-values-goals-and-preferences
Knowing when someone is in the last days and hours of life is not always easy. It is important to get the views of all those involved so that everyone is in agreement that the person is in the last days and hours of life and a death is expected.Informed about palliative and end of life care - NHS Education for Scotland (NES)
https://learn.nes.nhs.scot/3113/palliative-and-end-of-life-care-enriching-and-improving-experience/informed-about-palliative-and-end-of-life-care
Our resources will support adult social care staff, and their managers, to develop their skills and knowledge in end of life care.
https://www.skillsforcare.org.uk/Learning-development/ongoing-learning-and-development/end-of-life-care/End-of-life-care.aspx
Definition of End of Life Care
General Medical Council 2009
https://web.archive.org/web/20120504103457if_/http://www.gmc-uk.org/static/documents/content/End_of_life.pdf
People are ‘approaching the end of life’ when they are likely to die within the next 12 months.
This includes people whose death is imminent (expected within a few hours or days) and those with:
- Advanced, progressive, incurable conditions
- General frailty and co-existing conditions that mean they are expected to die within 12 months
- Existing conditions if they are at risk of dying from a sudden acute crisis in their condition
- Life-threatening acute conditions caused by sudden catastrophic events.
- Panduan ini juga berlaku untuk neonatus yang sangat prematur yang prospek untuk bertahan hidup diketahui sangat buruk, dan untuk pasien yang didiagnosis memiliki status vegetatif persisten (PVS), yang keputusannya untuk menarik perawatan dapat menyebabkan kematian mereka.
A QUICK GUIDE to Identifying Patients for Supportive and Palliative Care
http://www.cheshire-epaige.nhs.uk/wp-content/uploads/2018/11/A-Quick-Guide-to-Identifying-Patients-for-Supportive-and-Palliative-Care.pdf
Sekitar 1% dari populasi meninggal setiap tahun, namun secara intrinsik sulit untuk memprediksi atau mengidentifikasi pasien mana yang mungkin dalam tahun terakhir kehidupan mereka. Jika diprediksi sebelumnya, beberapa tindakan perawatan suportif dapat diperkenalkan yang akan memungkinkan diskusi lebih awal dari keinginan mereka, meningkatkan perawatan yang selaras dengan preferensi mereka dan lebih sedikit krisis.
Singkatnya, jika kita dapat mengidentifikasi pasien-pasien ini dengan lebih baik, kita mungkin akan lebih mampu memberikan perawatan yang lebih baik bagi mereka ketika mereka mendekati akhir hidup mereka.
The main processes used in GSF are to identify, assess, plan, and at all times communicate about patient care and preferences. Use of this guidance might enable better identification of patients nearing the end of their lives i.e. in the last 6-12 months of life, to trigger better assessment and pre-planning e.g. holistic needs assessment, Advance Care Plans, and the appropriate management care plan and provision of supportive care related to their needs.
https://web.archive.org/web/20101126173257/http://www.goldstandardsframework.nhs.uk/Resources/Gold%20Standards%20Framework/PrognosticIndicatorGuidancePaper.pdf
Decisions relating to Cardiopulmonary Resuscitation (3rd edition - 1st revision )
https://www.resus.org.uk/dnacpr/decisions-relating-to-cpr/
https://www.resus.org.uk/_resources/assets/attachment/full/0/16643.pdf
CPCRE - Centre for Palliative Care Research and Education
https://www.health.qld.gov.au/cpcre
GOOD PALLIATIVE AND END OF LIFE CARE
https://sites.google.com/view/palliative-care-resources/good-palliative-and-end-of-life-care
Start Your Palliative Care Education Today
https://palliativecareeducation.com.au/
Welcome to the Tasmanian Palliative Care Formulary
https://palliativecareformulary.tas.gov.au/SpecialtyFormulary/3
Palliative and end of life care services in Scotland
These indicators apply to all palliative and end of life care services in Scotland whether directly provided by an NHS board or secured on behalf of an NHS board and focus on:
- identification
- assessment and care planning
- accessing patient information, and
- place of death.
https://www.africanpalliativecare.org/
https://www.chpca.ca/
https://hospicecare.com/home/
https://www.nhpco.org/
https://palliativecare.org.au/
https://www.palliative.info/
https://www.ageuk.org.uk/
“What is a palliative care social worker and what do they do?”. It’s a question that gets asked regularly and is one that can elicit a variety of answers depending on the person being asked and the setting in which the role operates.
https://www.apcsw.org.uk/social-worker-role/
NHS Education for Scotland website aims to support healthcare staff who are working with patients, carers and families before, at, and after death. It provides key information on the clinical, legislative, and practical issues involved.
http://www.sad.scot.nhs.uk/
Best Practice ACP Principles
1. Adults are presumed to have capacity
2. Decisions are person-centred
3. Decision-making must reflect respect for life and the person’s right to personal autonomy
4. Quality of life is defined by the individual
5. Care should be multidisciplinary in nature to meet the individual needs of the person and their family
6. Health decisions may be broad and can relate to any time in the future
7. All efforts will be made to obtain the appropriate consent through a collaborative approach
8. Substitute decision-maker/s make decisions in the person’s best interests
9. Transparency and accountability for decision-making
10. ACP is more than planning for decisions about life-sustaining medical treatment at the end of life.
https://web.archive.org/web/20200320171629/https://www.health.qld.gov.au/__data/assets/pdf_file/0037/688618/acp-guidelines.pdf
Nausea and vomiting in palliative care
Ookay kan, Bro!